Salaamun Alaykum,
The Health Awareness Team will be e-mailing monthly 'Health Bulletins', which will include issues relating to health awareness, identifying symptoms and general updates. The purpose is to increase health awareness amongst our community members.
As always, we welcome any contributions of articles, suggestions of topics or your involvement in this and various other health awareness projects, please contact me on This email address is being protected from spambots. You need JavaScript enabled to view it.
Salaams and Duas,
Asif Alidina
Physical fitness and moral fibre: the inspiration for the modern Olympics
By Dr Abbas Ramji
Sixty-four years since London last hosted the most prestigious games on earth, during the summer of 2012 the capital of England yet again celebrated the awe-inspiring collation of sporting events that is known as the modern Olympics. Whether you are interested in the Olympics or not, it is an event that takes place every four years that is practically impossible to avoid. It not only is a merriment of sporting prowess, but represents all nations from across the globe, without exception, coming together peacefully to promote the qualities that sustain life itself, physical fitness and moral fibre.
London’s bid to host the Olympic games won favour from the International Olympic Committee at the expense of strong rival bids from other cities due to one pivotal pledge, the commitment to inspire the younger generation to partake in sport and in turn promote fitness intertwined with morality for generations to come, extending the games beyond the few weeks that they physically span across to a transformative continuum. This runs to the very core of the inspiration of the modern Olympics itself, the essence of why the Olympics were resurrected. When we reflect upon these Olympic pillars of promoting fitness and morality, we become conscious of how this mirrors our Shia Islamic religion. It is often discussed within the realms of our faith that we must work towards promoting our wellbeing, both physically and spiritually in order to optimise benefits of this world and the hereafter.
London’s Olympic Organising Committee ingeniously promoted the story of how the modern Olympics were enthused in a very subtle manner that may have escaped even the most discerning spectator. The 2012 Olympic mascot, a one eyed alien-looking blue creature was named Wenlock. Delving into the eye of Wenlock opens up the tale of a single minded English country doctor, William Penny Brookes, born in 1809 in Much Wenlock, Shrophire, England. Dr Brookes trained in surgery in London and also ironically in Paris, the unsuccessful rival Olympic city bidder, before returning to his home in the English Midlands to take over his father’s medical practice in 1831. As a self-fulfilled Victorian philanthropist, Dr Brookes immersed himself into building and developing his local community, having almost solitarily established the local school, improved the roads, introduced street lighting and brought railway to his town.
However, more than all these esteemed accomplishments, his true ambition was to revive the ancient Olympics. Dr Brookes set up the Wenlock Agricultural Reading society in 1841, and less than a decade later, an off shoot from this organisation was the Wenlock Olympic Society. This organisation devoted itself to staging an annual sporting event to “promote the moral, physical and intellectual improvement” of the town’s inhabitants, “especially of the working classes by the encouragement of outdoor recreation”. Perhaps it can be argued that this nineteenth century committee in the rural English countryside was the modern inspiration of outdoor physical games in schools across the world. Dr Brookes’ knowledge about premature deaths among weavers through a lack of outdoor exercise was recorded as his inspiration. He was well known for lobbying the British Government of the era to make physical exercise a compulsory element of the school curriculum, using evidence that he collected from Wenlock schoolboys that gymnastics improves physique. Likewise, our Jamaats across the world also aim to promote sports within our communities as a central activity. This not only promotes improved physical health of our communities, but contributes towards enhanced social cohesion, the essential ingredient for a successful community.
Utilising the ideals of the creativeness of ancient Greek athletics, the first games initiated by Dr Brookes were held in a field in the crisp English autumn of 1850 with the full pageantry and eccentricity of a village fayre. Sports included hurdles, running, cricket, football, cycling on penny farthings, blindfolded wheelbarrow races and even a race for “old women” to win a pound of tea. These games continue annually even today.
Dr Brookes’ sights were set beyond Much Wenlock to an international stage. He initially lobbied the local council until the Shropshire Olympic Games, a regional county-wide games were setup in 1861. Having then co-founded the British National Olympic Association, he helped establish Britain’s first national Olympics held in Crystal Palace, London in 1866. He continued his plight by diligently lobbying the Greek Government to reinstate the International Olympic games. This inspirational beacon who campaigned throughout his life for an Olympic games to promote physical fitness and moral fibre passed away weeks before the first modern Olympics opened in Athens in 1896. Using this year’s Olympic games, we as a global community must take inspiration from this individual to promote well-being and improved health among ourselves both individually and collectively. Regional sports tournaments are held among our community on a regular basis but perhaps they only attract a sector from within our community. The challenge now lies in how to modify these tournaments to promote on-going improved health throughout the year as a continuum and to also consider how such events can appeal to the wider community as do the Olympic games themselves.
Reference:
Moore W (2012). A doctor’s lifelong campaign to revive the Olympic games. BMJ, 344, 51.
The memory of water
By Dr Abbas and Dr Israh Tejani
"And among His Signs is that …He sends down water from the sky, and therewith revives the earth after its death. Verily, in that are indeed signs for a people who understand." (Holy Qur’an 30:24)
Water is a simple substance that is often taken for granted. Yet through its intricate properties, its existence allows life, as every living being in this world contains water. The human being is made up of 70% water, much like the world itself.
A theory was put forward in 1988 by Jacques Beneviste that water is capable of having a memory, a theory that was subsequently rigorously tested by hundreds of experiments, majority of which confirmed this hypothesis. Recently in Japan, Dr. Emoto performed an experiment where he put some normal tap water into several test tubes. He then said different words, blowing into a different test tube each time he had said a different word. He subsequently used an electron microscope to see the shape of the crystalline structure of the water in each test tube, and compared it to the pictures he had taken before. The results were astonishing, for the shape of the water changed depending on what word was said – it “remembered” the word. Other studies have shown that the shape of water can have a great impact on the body – a good shape can help restore or keep the body in a state of health, whilst a bad shape can lead to many diseases, one of which is cancer.
This idea is extremely relevant to some of the things we have been taught in Islam. As a child I was always taught the importance of saying “Bismillah” before eating or drinking anything. Dr. Emoto found that the word “God” transformed the water into a beautiful shape. As 70% of the human body is made up of water, and a lot of our foods contain water, saying “bismillah” before eating will help to change not only the crystalline shape of what we are about to consume into a nice, harmonious structure, but also help to refine the cells in our body, helping us become stronger against disease.
As I was growing up, I used to see my mother blow into a glass of water after reciting duas, something that is highly emphasised in Islam. We are sometimes even taught to wash ayaats of the Holy Qur’an and to drink this water. It is natural to question this practice, as at first sight it does not seem to make logical sense. However, the impact that reciting dua has on the shape of the water molecule was tested by Dr. Emoto. The pictures below illustrate his findings.

We see that after the dua was recited, the water changed into a beautiful, symmetrical shape. Through this, we can begin to understand why reciting du’as or the Holy Qur’an upon water can provide us with a cure. In fact, there has recently been much discussion and research regarding ‘digital biology.’ This is where waves are fired at a drug from a transmitter, and the scattering pattern of the waves is then collected at the receiver. The waves that are collected at the receiver are then fired at a glass of water, and the patient asked to drink it. A study conducted by Thomas found that treating a human breast tumour in mice with water that had been transformed in this way from the audio signal of Taxol® (usually used to treat breast cancer) showed just as much statistical significance as treating it with the drug itself (ie, it was just as beneficial as taking the drug itself)
It is only natural that we then turn and think about the events that took place on the 10th of Muharram. Hazrat Abbas (AS) took a handful of water from the Euphrates, looked into it and then threw it down. However, his influence upon the water was so great that the Euphrates now remains in constant circumambulation (tawaaf) around his grave. In addition to this, Dr. Emoto found that saying the word ‘peace’ over the water gave it an almost perfect shape. If we cast our minds back to the moment when Imam Hussain (AS) was delivering his last will to Imam Sajjad (AS), we realise the wisdom of his words when he said: “When my shi’a drink a cool glass of water, tell them to send me their salaam.”
In trying to look for the perfect crystalline structure of water, Dr. Emoto stumbled upon the perfect combination, which is love plus gratitude. Just one of these is not enough. Love needs to be based in gratitude, and gratitude needs to be based in love. The Holy Qur’an tells us time and time again to continue giving thanks for what we have, and we can now begin to see the wisdom behind that command. Sometimes, when we cannot see the immediate results of our prayers, we think that we have failed. But one thing that Dr. Emoto's photographs show is that the mere thought of failure itself becomes represented in the physical objects that surround us. Upon reading this short article, perhaps we can begin to realise that even when immediate results are invisible to the unaided human eye, they are there. When we love our own bodies, they respond. When we express our love to God and other fellow human beings, they respond. And now we have seen before our eyes the proof that water is far from inanimate – it is actually alive and responsive to our every thought and emotion. Perhaps, having seen this, we can begin to really understand the tremendous power that we possess, and through choosing our thoughts and intentions, we can heal ourselves and the earth. If only we believe.
“The cure is within you but you do not see. The illness is from you but you do not realise. Do you think you are but an insignificant mass, whilst within you lies a great universe?”-- Imam Ali (AS)
***********************************************************************************
Why Do We Cry? A Scientific Perspective
By Dr Abbas and Dr Israh Tejani
As the new Islamic year commences, we begin the year 1434 with days of mourning. Indeed, throughout the year, we are encouraged to mourn, be it during the days of shahadat or when repenting to Allah (SWT). Though we understand the spiritual benefits of crying, could it be that there are physical benefits to our bodies from the act of crying?
In science, we can broadly categorise tears into three main types: Basal tears, irritation tears and emotional tears.
Basal tears are the tears, or liquid, that coats our eye on a blink-by-blink basis. They contain antibodies and enzymes that defend against disease-causing microbes and bacteria that the eye encounters. Basal tears, like all tears, have numerous components. A little bit of mucus allows them to adhere to the eye surface without causing harm. The main part of a tear contains water and salts (like sodium chloride and potassium chloride). The ratio of salt to water in tears is similar to that of the rest of the body. If the body's salt concentration climbs too high, it will take advantage of these tears and increase the salt concentration within these tears.
Our eyes produce irritant tears when hit by wind or sand (or any other foreign body). Irritant, or reflex, tears have the same constituents as basal tears, and work toward the same goal: protecting the eyes. However, since they are designed to break down and eliminate eyeball-intruders like airborne dust, these tears tend to flow in greater amounts and contain a greater concentration of antibodies and enzymes that target micro-organisms. Thus, irritant tears are not just basal tears in greater quantity; different biological processes precede the excretion of the two types of solution.
The voluminous tears that so rapidly move us to frustration or pity are, of course, emotional tears and this is what most of this article will look at. Aside from the constitution of salt, water and enzymes, emotional tears have been found to also contain large amounts of hormones associated with stress. These hormones include prolactin, adrenocorticotropic hormone (ACTH), Leucine-Enkephalin and manganese. If these are not excreted at all, they would build up to toxic levels in the blood that could weaken the body's immune system and other biological processes. But here, as in other areas, the body has its own mechanisms of coping. We secrete stress hormones when we sweat and when we cry. Clearly, then, it is physically very healthy to cry, regardless of whether or not it feels awkward or embarrassing socially. When going through a stressful time or a bereavement, people frequently report feeling better after crying and this is doubtlessly connected to the discharge of stress-related hormones; some of the hormones excreted in tears are even associated with the experience of physical pain, rendering weeping a physiologically pain-reducing process.
Prolactin, is found in much higher concentration in women's bodies than in men's. Interestingly, prolactin appears to not only be secreted in tears but also to play a role in the formation of tears. Levels of prolactin in the body correlate positively with frequency of emotional crying; as a whole, women cry more often than men (perhaps four times as often, according to one study) and women also have a lot more prolactin than men (60% more). The levels of prolactin in one's system provide a threshold effect, affecting how easily emotional tears are shed in response to a given stimulus. The fact that men's tear glands are, as a whole, structurally smaller than women's supports the notion that they are used less – perhaps, therefore, one can argue that there is a physiological reason why women are more likely to cry than men.
Dr. William Frey, a biochemist in Minnesota, has researched the chemical content of human tears. One of the substances found in tears was the stress hormone ACTH. Shedding tears helps to reduce excessive amounts of ACTH and other substances that accumulate following a stressful event. Dr. Frey has suggested that the purpose of emotional crying may be to remove waste products from the body, similar to other excretory processes such as urinating, defecating, exhaling, and sweating. Frey's conclusion is that "we may increase our susceptibility to a variety of physical and psychological problems when we suppress our tears." Crying not only removes toxins from the body but also reduces tension.
Studies on adults in psychotherapy have found lower blood pressure, pulse rate, and body temperature in patients immediately following therapy sessions during which they cried and raged. Similar changes were not observed in a control group of people who merely exercised for an equivalent period of time.
A study was performed in Heidelberg, Germany, from 1973 to 1986 on the effects of both suppressing one’s grief and crying on patients’ long-term health. This study was carried out on 7,000 patients. The results showed that cancer and heart disease were most prevalent in the group who had suppressed their grief for two years or more and least frequent in the group who had no restriction on their amount of crying. This showed an almost protective effect of crying on developing these conditions.
Putting the science into an Islamic perspective
Countless studies (more studies than we have space to write about) have shown that crying in an emotional state not only acts as a psychological stress reliever, but also improves the biochemical composition of our bodies (i.e., it helps to make our bodies healthier at the microscopic level). In the Qur’an, Allah (SWT) emphasises the importance of crying in numerous verses, including one of the more well-known verses: “Indeed, Allah (SWT) loves those who repent.” (2:222).
When we now look at Muharram and Safar, we see that during these days, one is encouraged to reflect on the tragedies that befell Imam Hussain (AS) and his family and to shed tears in grief. When listening to the noble and heroic sacrifice of Imam Hussain (AS) and the brutal massacre of the family of the Prophet (SAW) our eyes cannot help but shed tears for Imam Hussain (AS). This not only helps us spiritually, but also confers a physical and physiological benefit to our bodies.
Through reading this article, one will realise that alongside the multitude of spiritual benefits that one can obtain from crying, be it in repentance or on the sacrifice of Imam Hussain (AS), there are also a huge number of physical benefits of crying. Indeed, not only has our Master Hussain (AS) given the ultimate sacrifice by laying down his life to protect Islam, through his martyrdom he has also created a means to improve our physical health through crying over his tragedy. We can now begin to understand what Imam Hussain (AS) meant in his final farewell to Imam Sajjad (AS) when he said: “When you return to Madinah and you meet my Shi’a, let them know that on the plains of Karbala, your Maula (AS) was remembering you tremendously.”
“Surely, there is a burning heat in the hearts of the believers with respect to the killing of Husain that will never cool down” – Imam Jaffar as-Sadiq (AS)
Depression
Depression is common. Symptoms can affect day-to-day life and can become very distressing. Treatments include talking treatments and antidepressant medicines. Treatment takes time to work but has a good chance of success. Some people have recurring episodes of depression and require long-term treatment to keep symptoms away.
What is depression?
The word depressed is a common everyday word. People might say "I'm depressed" when in fact they mean "I'm fed up because I've had an argument, or failed an exam, or lost my job" etc. These ups and downs of life are common and normal. Most people recover quite quickly.
With true depression, you have a low mood and other symptoms each day for at least two weeks. Symptoms can also become severe enough to interfere with day-to-day activities.
Who gets depression?
About 2 in 3 adults have depression at some time in their life. Sometimes it is mild or lasts just a few weeks. However, an episode of depression serious enough to require treatment occurs in about 1 in 4 women and 1 in 10 men at some point in their lives.
What are the symptoms of depression?
Many people know when they are depressed. However, some people do not realize when they are depressed. They may know that they are not right and are not functioning well, but don't know why. Some people think that they have a physical illness, for example, if they lose weight.
The following is a list of common symptoms of depression. It is unusual to have them all, but several usually develop if you have depression.
- Low mood for most of the day, nearly every day. Things always seem 'black'.
- Loss of enjoyment and interest in life, even for activities that you normally enjoy.
- Abnormal sadness, often with weepiness.
- Feelings of guilt, worthlessness, or uselessness.
- Poor motivation. Even simple tasks seem difficult.
- Poor concentration. It may be difficult to read, work, etc.
- Sleeping problems:
- Sometimes difficulty in getting off to sleep.
- Sometimes waking early and unable to get back to sleep.
- Sleeping too much sometimes occurs.
- Lacking in energy, always tired.
- Difficulty with affection, including going off sex.
- Poor appetite and weight loss. Sometimes the reverse happens with comfort eating and weight gain.
- Irritability, agitation, or restlessness.
- Symptoms often seem worse first thing each day.
- Physical symptoms such as headaches, palpitations, chest pains, and general aches.
- Recurrent thoughts of death. This is not usually a fear of death, more a preoccupation with death and dying. Some people get suicidal ideas such as ..."life's not worth living".
The severity of the symptoms can vary from mild to severe. As a rule, the more symptoms from the list above that you have, the more severe the depression is likely to be.
What causes depression?
The exact cause is not known. Anyone can become depressed. Some people are more prone to it, and it can develop for no apparent reason. You may have no particular problem or worry, but symptoms can develop quite suddenly. An episode of depression may also be triggered by a life event such as relationship problem, bereavement, redundancy, illness, etc. In many people it is a mixture of the two. For example, the combination of a mild low mood with some life problem, such as work stress, may lead to a spiral down into depression.
Women tend to develop depression more often than men. Particularly common times for women to become depressed are after childbirth (postnatal depression) and the menopause.
A chemical imbalance in the brain might be a factor. This is not fully understood. However, an alteration in some chemicals in the brain is thought to be the reason why antidepressants work in treating depression.
Some myths and other points about depression
Depression is common, but many people don't admit to it. Some people feel there is a stigma attached, or that people will think they are weak. Depression is one of the most common illnesses that GPs deal with. People with depression may be told by others to 'pull their socks up' or 'snap out of it'. The truth is, they cannot, and such comments by others are very unhelpful.
Understanding that the symptoms are due to depression, and that it is a common illness, may help to accept that you are ill and need help. This may be particularly true if you have physical symptoms such as headache or weight loss. Some people ask "am I going mad?" It may be a relief to know that you are not going mad, and the symptoms that you have are common and have been shared by many other people.
You may 'bottle up' your symptoms from friends and relatives. However, if you are open about your feelings with close family and friends, it may help them to understand and help.
What are the treatment options for depression?
In general, treatments are divided into those used for mild depression and those used for moderate and severe depression.
What if I don’t have any treatment?
Most people with depression would get better without treatment. However, this may take several months or even longer. Meanwhile, living with depression can be difficult and distressing (and also for your family and friends). Relationships, employment, etc, may be seriously affected. There is also a danger that some people turn to alcohol or illegal drugs. Some people think of suicide. Therefore, many people with depression opt to try some form of treatment.
Treatment options for mild depression.
In general, mild depression means that you have some of the symptoms listed above, but are still able to cope reasonably well with normal activities. For example, you may still be able to do your normal job, and get by with household chores, but perhaps with difficulty. Your doctor may suggest one or more of the following.
- Talking treatments (psychological treatments).
- Specific counselling (following marital problems; bereavement; childhood abuse; etc).
- An exercise programme (regular exercise programme, 3 times per week, for 12 weeks).
- A self-help programme.
- Antidepressant medicines.
It is best to discuss the treatment options with your doctor, who will be able to advise you of the best treatments options for you.
Treatment options for moderate or severe depression.
In general, moderate depression means that you have several of the symptoms listed above, and you find great difficulty in coping with normal activities. Severe depression is even worse. In these situations, a doctor may suggest one or more of the following.
- Antidepressant medicines.
- Talking (psychological) treatments.
It is best to discuss the treatment options with your doctor, who will be able to advise you of the best treatments options for you.
Some dos and don'ts about depression
- Don't bottle things up and 'go it alone'. Try and tell people who are close to you how you feel. It is not weak to cry or admit that you are struggling.
- Don't despair - most people with depression recover. It is important to remember this.
- Do try and distract yourself by doing other things. Try doing things that do not need much concentration but can be distracting such as watching TV. Radio or TV is useful late at night if sleeping is a problem.
- Do eat regularly, even if you do not feel like eating.
- Don't make any major decisions whilst you are depressed. It may be tempting to give up a job, or move away, to solve the problem. If at all possible you should delay any major decisions about relationships, jobs, or money until you are well again.
- Do tell your doctor if you feel that you are getting worse, particularly if suicidal thoughts are troubling you.
- Sometimes a spell off work is needed. However, too long off work might not be so good as dwelling on problems and brooding at home may make things worse. Getting back into the hurly-burly of normal life may help the healing process when things are improving. Each person is different, and the ability to work will vary.
- Sometimes a specific psychological problem can cause depression, but some people are reluctant to mention it. One example is sexual abuse as a child leading to depression or psychological difficulties as an adult. Tell your doctor if you feel something like this is the root cause of your depression. Counselling may be available for such problems.
Hookahs
|
 |
Definition and usage
Hookahs, also known as narghiles, shisha or hubble-bubble pipes have long been used for smoking tobacco in the Middle East and parts of Africa and Asia.
Hookah smoking is often a social activity and two or more people may share the same pipe. In some cultures, children may smoke with their parents. Although their usage appeared to be declining by the mid 1980’s, more recently there has been an upturn in their popularity in the eastern Mediterranean region and hookah cafes and bars are also beginning to appear in North America, Brazil and Europe. A study of Parisian schoolchildren found that more than half of 16 year olds had tried shisha once and 25% reported smoking it occasionally.
Hookahs’ smoking appears to be particularly popular among students and young people who enjoy the novelty and conviviality of sharing the Hookahs, although in some countries many young people appear to be even unaware that it contains tobacco.
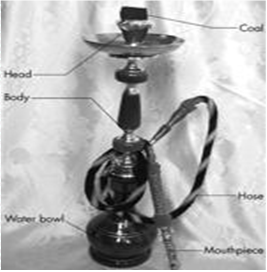
What are Hookahs?
Hookahs generally consist of a head, body, water bowl and hose. Tobacco, which may be flavoured with fruits and sugar syrup, is placed in the head and often covered with perforated Aluminium foil. Burning charcoal is placed on top of the foil. Water is placed in the bowl, submerging a tube through which smoke leaves. Sucking on the hose causes a vacuum in the air space above the water, causing smoke to pass through the water producing bubbles (hence the common name “hubble-bubble”). Disposable mouthpieces may be attached to the end of the hose to reduce the risk of infection. The size of the Hookah, number of hoses and other features may vary.
Health Impact
Because the smoke passes through the water before the smoker inhales it, there is a common misconception that the water “filters out” the harmful substances in tobacco smoke. Also the use of herbs or fruits as flavourings masks the harshness of the tobacco, leading some users to believe that they are smoking a herbal product that appears less hazardous than conventionally smoked tobacco products. However, Hookah tobacco smoking delivers nicotine and as is common with other tobacco products, frequent use is associated with users reporting that they are addicted.
Furthermore, even after it has been passed through water, the smoke from a Hookah contains high levels of toxic compounds including carbon monoxide, heavy metals, and cancer-causing chemicals.
Although Hookah smoking has not been as extensively researched as cigarette smoking, preliminary research suggests that it is associated with many of the same risks as cigarette smoking and may incur some unique health risks. Nicotine dependence may also result from repeated inhalation of smoke from a Hookah since users receive comparable or higher doses of nicotine compared to cigarette smokers.
A laboratory based study compared exposure to Hookah toxicants with cigarette smoking among 31 participants aged between 18 and 50. Each person completed two 45-minute sessions, one in which they smoked tobacco using a Hookah and the other in which they smoked a single cigarette. The level of nicotine and carbon monoxide was measured in the participants’ blood, as was heart rate, puff number and puff volume. The researchers found that on average, expired air carbon monoxide levels increased by 23.9 parts-per-million for Hookah use and 2.7 parts-per-million for cigarette smoking. Peak nicotine levels did not differ significantly between use of Hookahs or cigarettes but carboxyhemaglobin* levels were three times greater after use of the Hookah than that observed after smoking a cigarette.
Short term health effects
After 45 minutes of Hookah use, expired air carbon monoxide, plasma nicotine and heart rate are substantially increased. Thus Hookah usage is likely to exert a similar cardiovascular response to that of cigarette smoking.
Longer term health effects
Whilst the health impacts of Hookah usage appear to be at least as comparable to those of cigarette smoking, research is complicated by the fact that many users are also cigarette smokers. However, evidence suggests that Hookah usage is likely to increase the risk of cancers of the lung, mouth and bladder. It is also associated with markers for cardiovascular disease and respiratory disorders.
Hookah users appear to be at increased risk of mouth and gum disease. A study in Saudi Arabia found that the relative risk for periodontal disease increased by 5-fold and 3.8-fold in Hookah and cigarette smokers respectively, compared to non-smokers. Sharing a Hookah mouthpiece also poses a serious risk of transmission of communicable diseases, including tuberculosis and hepatitis.
Secondhand smoke from Hookahs
The smoke from Hookahs is a mixture of tobacco smoke exhaled by the smoker plus smoke from the fuel used to heat the pipe, thus posing a serious risk to the health of non-smokers.
Children are particularly vulnerable to the effects of passive smoking. Because they spend a considerable amount of time at home, they may be at risk for Hookah smoke exposure in homes where such devices are used. A survey in Syria found that almost half (48.4%) of heavy users (those who smoked at least once a day) did so mainly in the home. New research has shown that a single Hookah use session emits in the side stream smoke approximately four times the carcinogens, four times the volatile aldehydes and 30 times the Carbon Monoxide** of a single cigarette. The authors conclude that, given a habitual smoker smoking rate of 2 cigarettes an hour, during a one-hour Hookah use session a Hookah smoker is likely to generate ambient carcinogens and toxicants equivalent to 2-10 cigarette smokers.
Public policy implications
Although research into the health impacts of prolonged Hookah usage is still in its infancy, there is now enough evidence of its harm to include Hookah smoking in public smoking bans. In countries where there is a tradition of using Hookahs, work to change cultural norms and attitudes will be required alongside any proscriptive laws and regulations. However in countries where Hookah usage is still a novelty, public health advocates should seize the opportunity to limit its spread through a combination of education and legal measures. Laws to ban or restrict smoking in public places should be drafted to ensure that Hookahs are covered by the relevant legislation. Hookah use in enclosed public places in the United Kingdom has been prohibited since July 2007.
| *Carboxyhemoglobin (COHb) is a stable complex of carbon monoxide and hemoglobin that forms in red blood cells when carbon monoxide is inhaled or produced in normal metabolism. Large quantities of it hinder delivery of oxygen to the body. Tobacco smoking (through carbon monoxide inhalation) raises the blood levels of COHb by a factor of several times from its normal concentration. |
| ** Carbon monoxide (CO) is a colorless, odorless, and tasteless gas that is slightly lighter than air. It is toxic to humans and animals when encountered in higher concentrations, although it is also produced in normal animal metabolism in low quantities, and is thought to have some normal biological functions. In the atmosphere it is spatially variable, short lived, having a role in the formation of ground-level ozone. |
Stop smoking: The benefits and aids to quitting. (Part 1)
- Introduction
- The desire to stop smoking
- Increase in life-span
- Health benefits
- Smoking cessation aids
Introduction
This sheet reviews the health benefits of stopping smoking and aids to Quitting. Stopping smoking is always beneficial to heath and it is never too late. Every cigarette smoked damages the lungs in a way that may not show up until later in life. After the age of 35-40 years, for every year of continued smoking a person loses 3 months of life expectancy. Many smokers think that they will be more miserable when they stop but the evidence is that they will have better mental health and be happier.
The desire to stop smoking
Many smokers continue smoking not by choice but because they are addicted. A large part of this addiction arises from dependence on the nicotine delivered. Addiction does not make it impossible to stop doing something, it just means that there are powerful urges and needs that have to be overcome in order to do so. Anything that can strengthen the resolve to resist these urges and needs or reduce their frequency or intensity can help in overcoming the addiction.
It is not clear why some attempts to stop succeed and others do not, though smoking fewer cigarettes per day, not needing to smoke first thing in the morning and not suffering from mental health problems or other addictions are favourable factors for success.
Increase in life- span
Two major longitudinal studies have demonstrated the benefits of stopping smoking at an early age. The 50 year follow up of the British doctors’ study revealed that if smokers quit before the age of 30 they can avoid more than 90% of the smoking-attributable risk of lung cancer. The authors concluded that stopping smoking at age 60, 50, 40, or 30 gains, respectively, about 3, 6, 9, or 10 years of life expectancy.
Health benefits after stopping smoking
Some of the health benefits from stopping smoking can occur quite quickly as the table below shows. Other health improvements are seen over the course of a number of years, depending on how long a person has smoked.

Source: Smokefree NHS website.
Switching to othertypes of tobacco: pipes, cigars and shisha
Some smokers switch to pipes or cigars in the belief that they are less dangerous forms of smoking. However, there is no safe level of use of any tobacco product. Some smokers may incur the same risks as smoking cigarettes and may even increase them, especially if they inhale the pipe or cigar smoke.
Similarly, waterpipes (also known as shisha or hookah pipes) are potentially just as hazardous as smoking other forms of tobacco.
Switching to other sources of nicotine
Electronic cigarettes are increasing in popularity as an alternative to conventional smoked tobacco products but there is currently little research and no official guidance on their safety in the United Kingdom. Furthermore there is no clear evidence yet that e-cigarettes are effective as a stop smoking aid although survey data suggests that about 4 in10 users do utilise them in an attempt to quit smoking. A decision on the regulation of e-cigarettes is expected to be made by the Medicines and Healthcare products Regulatory Agency (MHRA) in May 2013. The World Health Organisation is also expected to publish guidance on e-cigarettes in 2013.
Smoking cessation aids
There are many things that smokers can do to improve their chances of quitting. These falls into two categories: medication and psychological support.
Medication
Medications aim to help smokers quit smoking by reducing the chemically-driven need to smoke and/or blocking the pleasure associated with smoking. Nicotine Replacement Therapy (NRT) works by replacing the nicotine provided in cigarettes and allowing smokers to slowly reduce their dependence on nicotine. Varenicline (Champix) works by alleviating nicotine withdrawal and reducing the “rewards” of smoking. There is evidence to suggest that using a combination of NRT medications (e.g. combining the nicotine patch with gum or lozenges) is more effective than using them in isolation.
Surveys consistently find that a majority of smokers want to quit.
In 2008, 68% of current smokers in Great Britain reported that they wanted to quit, with 22% saying they would very much like to give up and a further 23% saying they wanted to stop “quite a lot”. 83% of respondents gave at least one health reason for wanting to stop smoking. The cost of smoking was the next most common reason people gave for wanting to quit with 31% saying smoking was too expensive and a waste of money.
Stop smoking: The benefits and aids to quitting. (Part 2/2)
- Medication
- Behavioural support
- Unproven aids to cessation
Medication
Nicotine replacement therapy (NRT)
Nicotine replacement therapy (NRT) includes nicotine chewing gum, patches, lozenges, mouth spray, inhalator and nasal spray and is usually taken for 8 to 12 weeks.
NRT products can be purchased from a pharmacist and in some shops or obtained on prescription from a GP or qualified NHS Stop Smoking Advisor.
NRT is designed to reduce the motivation to smoke by replacing nicotine from cigarettes.
By alleviating nicotine withdrawal symptoms, the transition from cigarette smoking to complete abstinence is easier. Clinical trials have consistently found that NRT increases the success of quitting smoking by 50– 70%.
The National Institute for Health and Clinical Excellence (NICE) recommends that smokers who are committed to quitting should be offered NRT to support their quit attempt and that more heavily addicted smokers may be offered a combination of NRT products if required.
There is a commonly held belief amongst many smokers that nicotine causes cancer and that NRT is therefore also unsafe. But it is the tar in cigarette smoke along with other toxins which causes lung cancer and other smoking- related illnesses. Some smokers express concern about becoming addicted to NRT. However, this is rare, a better alternative to smoking, and in studies looking at NRT use for up to five years there have been no health concerns.
Varenicline (Champix)
Varenicline (Champix) is a prescription only medication which comes as a course of tablets lasting 12 weeks, sometimes with the option of a further 12 weeks for those that are not smoking at the end of the initial treatment. Varenicline works by preventing nicotine from reaching nicotine receptors in the brain which make cigarettes less satisfying.
Bupropion (Zyban)
Bupropion (Zyban) is a prescription-only medication which comes as a course of tablets lasting around 8 weeks. It does not contain any nicotine but works by reducing (or entirely alleviating) cravings and nicotine withdrawal by blocking the pleasure smokers feel when using tobacco. Bupropion is safe for most healthy adults but there are some documented side effects including insomnia, dry mouth and headaches.
Behavioural support
Behavioural support aims to strengthen the smoker’s motivation not to smoke and advise on ways on avoiding, escaping from or minimising urges to smoke with simple practical strategies.
Specialist Stop Smoking Practitioners
Most Stop Smoking Services offer closed groups, ‘rolling’ groups and drop-in sessions as well as individual appointments, facilitated by fully trained advisors. Clinical trials have found that stop smoking groups double a smoker’s chance of quitting successfully. There is some evidence that groups are more effective than individual counseling.
Most smokers attending groups will also use medication to maximise their chances of success.
For details of your local Stop Smoking Service, please see the NHS Smokefree website (http://smokefree.nhs.uk).
Community Stop Smoking Practitioners
Most GP surgeries, pharmacies, hospitals, midwifery services and mental health facilities will provide a free Stop Smoking Advisor to assist smokers who wish to quit. Clinical trials have found that one-to-one support doubles a smoker’s chance of quitting successfully. The majority of smokers seeing an advisor will also use medication to maximise their chances of success.
Telephone support
The National NHS Stop Smoking Helpline (0800 022 4 332) is a free service for smokers who wish to stop smoking but do not require the more intensive support offered by the Stop Smoking Services. In addition to this, some NHS Stop Smoking Services will provide psychological support over the telephone for smokers who are mobility impaired or unable to attend face to face services.
QUIT is a national charity with a free-phone number for smokers who would like telephone support. QUIT provides advice in a number of languages. Clinical trials have found that this kind of support can help smokers to stop.
Unproven aids to stopping smoking
The above quit smoking programmes have been evaluated in controlled clinical trials in which success rates in smokers using the aid have been compared with similar smokers using a placebo, nothing or something else. There are a number of commercial companies selling materials, devices and treatments, often claiming higher levels of effectiveness, which have not be evaluated in this way. Success at stopping smoking is somewhat unpredictable and many people will report having succeeded after using one of these treatments but unless the aid has been subjected to comparative trials that are either independent of the company or audited by an independent agency, smokers would be advised to treat claims of effectiveness with caution.
The Health and wellbeing committee will be organising a Carbon Monoxide (CO) breath test for all members on Thursday 23rd May 2013 after the program. More details on this will be announced during the forthcoming jamaat programs.
Questions & Answers
- What does a CO breath test show?
It shows the amount of carbon monoxide (ppm CO) in the breath, which is an indirect, non-evasive measurement of blood carboxyhemoglobin (%COHb).
- What does ppm mean?
Parts Per Million. It is a unit of measure. In this case, one part CO in one million parts air (breath).
- How does smoking elevate COHb?
In a typical puff of a cigarette smoke there is about 5% CO by volume. This will compete with oxygen very successfully to form COHb (combination of CO and blood). This will eventually be excreted via the lungs; the same way it went in.
-
What else does breath CO show?
It acts as an indicator as to the possible level of some 4000 toxic substances in cigarette smoke, some 60 of which cause cancer. - How quickly does the CO disappear from the body after smoking stops?
It takes about 5 to 6 hours to reduce the original level by a half. Usually after a maximum period of 48 hours the ex-smoker would show the level of a non-smoker living in the same environment. - How long after a cigarette should the test by conducted?
More than 10 minutes. - What levels of breath CO do you expect to see?
• 0-6 non-smoker
• 7-10 light smoker
• 11-20 smoker
• 20+ heavy smoker
Thalassaemia
Pre-marital screening advice
It is important to think about various aspects prior to selecting a spouse. We tend to focus on these including the person themselves, their character, family and if they are compatible with us. One area often ignored is health, and specifically genetics. It is important to also take this into account as it has an effect on the children born following this marriage and impact on the family as a whole.
What are the threats faced within our community?
There has been a lot of discussion about genetics and cousin marriages in the past particularly surrounding the issue of Thalassaemia. Having looked at the recent evidence, it is clear that Thalassaemia is a threat to our community as we estimate that 9 in every 100 people carry the gene for Thalassaemia in our community. This is based on data over the last 20 years collected by the Medical Advisory Board of the World Federation. This is significantly higher than the population rate of 3 in every 100 (in the UK). The risk is also increased by the following factors:
- Small gene pool- there is only ~150,000 khojas in the world and most marriages take place within the community. This increases the likelihood of 2 carriers meeting in matrimony.
- Cousin Marriages- Though rare, cousins, especially first cousins can share up to 12% of their genes hence increasing the chances of genetic disorders to offsprings significantly.
- Ethnicity- A number of studies shows that Thalassaemia is linked to ethnicity and genetics disorders are generally higher in Asian ethnic groups. It is also thought to have a higher rate in areas of malaria prevalence such as East Africa as it has a protective feature.
Thalassaemia carriers (Thalassaemia minor) are often well and not aware of their carrier status unless they have been tested. This requires a simple blood test. Thalassaemia is only inherited and not caught and only those with both recessive genes (Thalassaemia Major) are ill from birth and need medical treatment such as blood transfusions on a routine basis. They also suffer from other complications such as frequent infections, iron overload needing painful overnight medication drips, increased risk of HIV and hepatitis B and so on. It also affects the families and the community at large apart from the cost of frequent treatment and suffering of the affected child.
All this is easily prevented by having a blood test to find the carrier status of both prospective spouses and avoiding a marriage between 2 carriers as it leads to a 1 in 4 chance of Thalassaemia major for each pregnancy. Marriage between a carrier and no-carrier is fine as there are no chances of having a Thalassaemia Major Child.
The second threat is that faced by the general population in regards to HIV and blood bourne viruses such as hepatitis B and C. These viruses can be deadly and even though there is effective treatment for HIV, Hepatitis B & C has no effective cure. They are transmitted sexually and via blood transfusions and the infection rates are higher than ever. It is important for each prospective spouse to safeguard themselves against such infections and there should be no taboo in asking for these tests to be carried out for both the boy and the girl by their families. In fact, it should be common practice as I am sure that each family values their child and want to make sure that they don’t get exposed to such infections.
What is Pre-marital Screening and why is it important?
Pre-marital screening is a basic health check which is done prior to a marriage to safeguard the couple and to give them enough information to make future informed reproductive choices. It requires each partner to undertake a test for a full blood count, iron levels and a haemoglobinopathy (Thalassaemia) tests together with a HIV test as a minimum. Other tests such as hepatitis screen and other genetic conditions common in the families can be added where necessary.
It is important as it provides a safeguard against sexually transmitted infections and enables the couple to make informed reproductive choices.
How can I be tested?
Testing can be done via your family doctor or a local clinic anywhere in Europe. In some cases, the tests are free and confidential. They don’t affect the premiums for insurances and are not disclosed to insurance companies. HIV tests are routinely done on many patients with severe infections, illness and in pregnancy.
Patients from abroad (not from Europe) can be tested privately at a small cost and most Jamaats have a local set up which they can advice you about.
What about the ethics surrounding such screening?
There has been several discussions regarding the ethics surrounding such testing. In the COEJ region, it was concluded that all Jamaats will provide facilities to check that such testing has been done prior to a nikah or will
expect both the bride and groom to obtain enough information via the Jamaat about the screening so that they are making an informed choice if not being tested. The jamaat expects the couple to share the results between them without disclosing it to the jamaat officials or their families if they choose to do so. There are 3 issues around ethics which have been considered:
- Confidentiality- We don’t plan to see the results of the tests but request that a certificate that the test has been carried out is given to the Jamaat officials prior to the marriage. The Jamaat official will ask the families if they are satisfied the results have been shared and that they understand the results and its implications.
- Right of refusing testing- The bride and /or the groom have the right to refuse testing. In any such event, the Jamaat will provide information as to why it is important to be tested and may ask the bride and groom to sign a disclaimer that they choose not to be tested and that they have been educated on the risks of not testing but choose to do so.
- Impacts to future Insurance- Under current legislation, results of genetic tests or negative HIV test is often not disclosed to Insurance companies and are not considered in the risk assessment process.
Please find below a leaflet on Thalassaemia which highlights the risks and some medical information about this condition. Should you need any further information, please email This email address is being protected from spambots. You need JavaScript enabled to view it. or This email address is being protected from spambots. You need JavaScript enabled to view it..
![]() Information leaflet on Thalassaemia.
Information leaflet on Thalassaemia.
Ramadhan Health Guide
 Ramadhan in the UK , is going to be very long! So, make sure you have read up on the Healthy Ramadhan Guide, identifying what foods to eat and what to avoid, and what foods release energy slowly throughout the day, helping you to 'manage' your fasts.
Ramadhan in the UK , is going to be very long! So, make sure you have read up on the Healthy Ramadhan Guide, identifying what foods to eat and what to avoid, and what foods release energy slowly throughout the day, helping you to 'manage' your fasts.
You can find the guide, which is written by UK Doctors and Health Consultants, promoted also by the NHS , on the following link where you can download it :